Mixing opioids with sedatives into poison cocktails has sparked a fatal "toxicity crisis" in Simcoe County, says a local public health nurse.
It’s a term she’s come to use after seeing a constant stream of alerts identifying new substances found in the unregulated drug supply, which now sees opioids combined with sedatives for longer effects and comes with a higher likelihood of poisoning.
Most recently, lab testing has shown the presence of medetomidine/dexmedetomidine combined with opioids in Toronto’s unregulated drug supply, which inevitably will make its way here, says Cathy Eisener, a public health nurse with the Simcoe Muskoka District Health Unit’s substance use and injury prevention program.
Medetomidine is a tranquilizer approved for use on animals by veterinarians, and dexmedetomidine (a more concentrated version of the sedative) is given to animals and people for sedation and pain relief. Typically, it is only used on patients in intensive care units, and tends to be an expensive drug.
It’s no longer accurate to say people are overdosing on unregulated drugs, says Eisener, who refers to these situations as drug poisonings. Often, people are taking very small amounts of a drug, unsure of its effect, and still experiencing poisoning. An overdose implies an intentional act of taking a lot of a drug, she explained.
“It’s not the same as when we were talking about things in 2017 … things have changed dramatically,” said Eisener. “We’re talking about people who have been so gravely impacted by the changes in the unregulated drug supply … these are people that deserve compassion and their family and their friends and everyone has been impacted.”
Since an unregulated drug supply is, as the name suggests, unregulated, Eisener and others in harm prevention and substance use support work have seen the supply go from a “drug” to a cocktail of drugs packaged into one substance.
Part of the reason is a pursuit of a longer high.
Heroin, said Eisner, might be taken two or three times a day to maintain the feeling it gives someone who uses it. But fentanyl stays in a human system for a shorter time, requiring more frequent doses to maintain the effect, she explained.
“So folks are adding the pieces like benzodiazepine, xylazine, and now the medetomidine … these things kind of enhance the effect of the fentanyl,” said Eisner. “Kind of like if you have a really bad headache and you take a Tylenol and a gravol.”
Benzodiazepine, xylazine and medetomidine are all sedatives, so a person who is taking opioids with these drugs mixed in often falls unconscious.
“We’re also seeing many different opioids within the unregulated supply … so it’s a cocktail of different things,” said Eisener.
Dr. Greg Devet, the chief of the emergency department at Collingwood General and Marine Hospital, said constant changes in the unregulated drug supply make treatment challenging.
“When patients do overdose, most fatalities occur in the field, many patients don’t even make it into the hospital,” said Devet. “For patients that do make it to the hospital … we may never know what exactly was in their bloodstream or their body.”
Emergency room medical staff administer naloxone to reverse the effects of opioids, which may or may not work; generally, they observe patients, hoping and waiting for the drug to clear from their system.
While the opioid effect can be reversed temporarily by naloxone (a standard response to a suspected opioid poisoning) the effects of the sedatives are not impacted.
“The unknowable nature of the drug supply … makes illicit drugs often very dangerous,” said Devet.
Some people are trying to make that unknowable nature a little more known.
Toronto's Drug Checking Service is one of the services offered through supervised consumption sites in Toronto, allowing those using unregulated drugs to bring a sample to the site to be analyzed and sent to a lab for testing to determine what chemicals and drugs are in the supply.
Some of the testing is done at the Centre for Addictions and Mental Health (CAMH) lab, under the direction of Dr. Christiana Stefan, a clinical biochemist and toxicologist.
“The more you know about what the unregulated drug supply contains, the better you can prepare … it’s part of a harm reduction strategy… it’s a way of empowering people who use drugs, also,” said Stefan.
For more than five years, the CAMH lab has been testing samples of drugs being sold illegally in Toronto and finding more and more “ingredients” in these drug cocktails.
The process used at the CAMH labs is liquid chromatography coupled with mass spectrometry, which separates the substances in the unregulated drug supply into “peaks” that can be recognized in the lab.
Stefan compares it to taking a tightly packed crowd of people and separating them so it’s easy to recognize who’s in the crowd. Regularly, there’s a "stranger" in that crowd.
This is what happened between Dec. 29, 2023 and Jan. 23, 2024 when the CAMH lab first spotted medetomidine in samples brought in through Toronto’s Drug Checking Service. By comparing the finding to chemical databases, the lab unmasked the "stranger" as medetomidine and/or dexmedetomidine.
With about 11 per cent of samples tested earlier this year containing medetomidine/dexmedetomidine, it’s considered a trend — not an isolated finding.
Though it's known in the veterinary and hospital crowds, the sedative is new to the unregulated drug supply crowd.
“It’s a new finding, but not a new discovery,” said Stefan, noting it’s an important distinction since it gives those responding to drug poisoning or supporting the unregulated drug supply users a head start in knowing what they can expect and how to treat it."
This fact separates medetomidine/dexmedetomidine from one of the other sedatives that found its way into the unregulated drug supply: xylazine.
Xylazine, explained Stefan, wasn’t approved for use in humans because of harmful side effects, and yet it was found in samples brought to Toronto’s Drug Checking Service in 2020.
Some of the effects of xylazine in humans include depression of the central nervous system (blurred vision, disorientation, dizziness, drowsiness, difficulty moving, slurred speech and fatigue), shallow or stopped breathing, low blood pressure, slower heart rate and painful open skin ulcers or abscesses prone to infection. The drug has also been fatal for humans.
The side effects of medetomidine/dexmedetomidine, when prescribed and taken at doses calculated by pharmacists and doctors, can include increased blood pressure followed by low blood pressure, hypothermia that doesn’t respond to conventional treatments, dry mouth, excessive sweating, nervousness, agitation, deep state of unconsciousness, slowing of heart rate and breathing, dilated pupils, and muscle twitching.
Sedatives have been identified in opioids sold on the street before 2020 as well.
Since 2018 when the CAMH lab started testing drugs brought into Toronto’s Drug Checking Service, tests have shown the addition of novel benzodiazepine, which have a range of effects from heavy hypnosis, sedation, amnesia, anti-anxiety, muscle relaxing, euphoria, loss of control and severe withdrawals.
There’s no way for someone taking a drug cocktail that contains medetomidine/dexmedetomidine, xylazine, and/or a benzodiazepine to know if the dose is appropriate or safe, which could result in more harmful side effects.
“The concern we have with any drugs that are used in an unregulated way, not in a prescribed way, or in an illicit way, if you will, is there is no drug without side effects,” said Stefan. “There is no drug that shouldn’t raise concerns when used inappropriately, and it just speaks to how the drug landscape continues to change and surprise us.”
There are no drug-checking services in Simcoe-Muskoka. Eisener explained the service is often tied to a consumption site because both require exemptions from the law governing controlled drugs and substances in Canada.
“It’s costly to have those services, but they can make a tremendous difference to folks,” said Eisener, noting she’s heard anecdotal evidence from people who chose not to use a drug after finding out what was in it. “From a harm reduction perspective, it’s really important to have drug checking.”
Though the samples that contained medetomidine/dexmedetomidine were from Toronto, Stefan said it’s fair to say the unregulated drug supply outside of Toronto likely also includes the sedative.
“We wouldn’t be surprised,” she said.
Eisener concurs, noting the unregulated drug supply makes its way up the 400 corridor and into Simcoe County and Muskoka communities.
“We have no way of confirming, but we often get reports back from our partners about what they’re seeing in the community,” said Eisener, adding there are observations from first responders about drug poisonings looking different and medical staff struggling to maintain a patient's breathing and having to do more chest compressions — likely the result of sedatives mixed with opioids.
Eisener said the suppression of breathing and heart rate is concerning, particularly because that’s also a side effect of opioids.
“The other thing is the prolonged sedation,” said Eisener.
Without knowing the dose of medetomidine/dexmedetomidine in a drug that’s been ingested, it’s impossible to know how long the sedation will be, but Eisener said she’s hearing it can last about 18 hours.
If someone is sedated for that long and not under medical care, problems like nerve damage can occur if the person is lying on one or more of their limbs, they can urinate or defecate while sedated and will be lying in it for hours, they can freeze without knowing it, and they can rouse temporarily and fall into more dangerous situations (like traffic or cold water) when they go unconscious again, she explained.
Eisener also points out the opioids have often worn off by the time a person wakes up from sedation, so they might be “dope sick” which leads to disorientation among other harmful effects.
Neither Stefan nor Eisener could predict where the unregulated drug supply would be looking for its next cocktail ingredient, but the current trends are worrying enough, and highlight the need for harm reduction.
Eisener hopes Barrie will soon get a supervised consumption site, and maybe, one day, a drug-checking service.
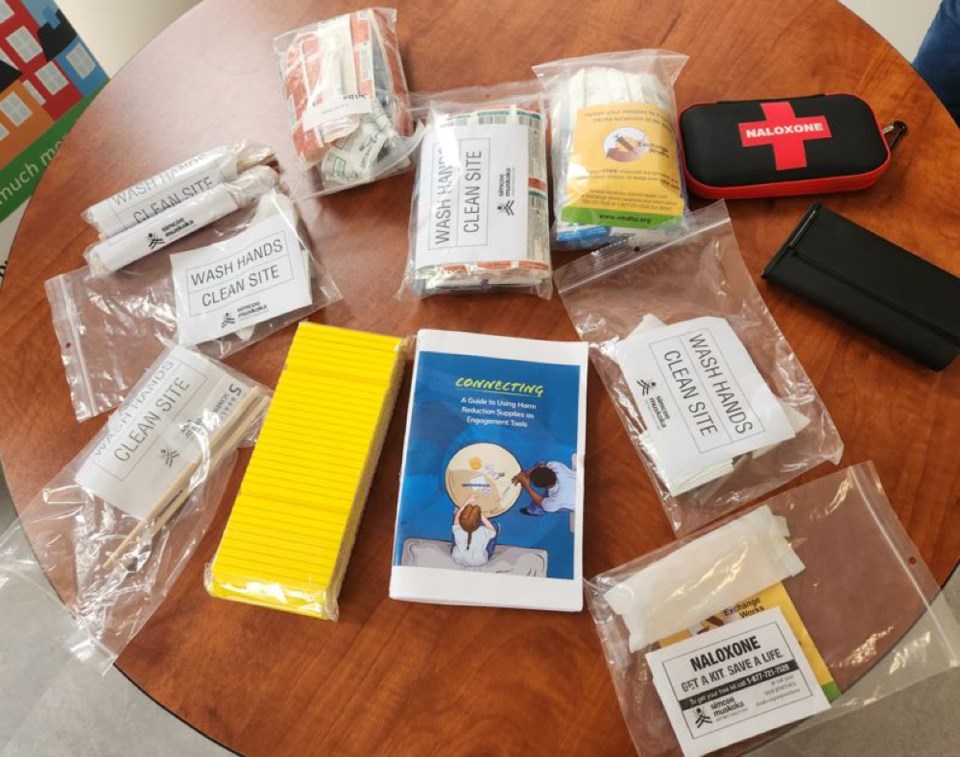
The health unit and CAMH recommend that people who use drugs follow precautions to avoid poisoning and/or to reduce the harm that could come from poisoning.
They include:
- Try a smaller amount of a drug, particularly if it looks different or was obtained through a different souces, and increase slowly if needed.
- Carry and be trained to use naloxone (also called Narcan) which is a drug that can temporarily reverse an opioid overdose. It is available free from pharmacies.
- Get your drugs checked through a drug checking service in Toronto at Moss Park Consumption and Treatment Service, Parkdale Queen West Community Health Centre, South Riverdale Community Health Centre, and The Works at Toronto Public Health (There are no sites in Simcoe County.)
- Use at a supervised consumption site or overdose prevention site. (There are no sites like this in Simcoe County.)
- Have someone with you when you are using and take turns spotting for each other.
- If you must use alone, let someone know before you use, and call the National Overdose Response Service at 1-888-688-6677 or download the Brave App on your phone.
- Call 911 in an overdose/ poisoning situation
- If your drugs didn’t contain what you were expecting, talk to the person you got your drugs from or get them from a different source.